Highlights:
- Many patients deferred care during the COVID-19 pandemic.
- Those choices will impact patients, providers, and payers in the coming years.
- It is expected that treatment will be more expensive going forward, and that scheduling healthcare may be more challenging than it was pre-COVID.

Many people chose to delay healthcare in the wake of COVID-19 concerns. Delays were sometimes recommended or requested by providers as well. This deferred care creates a significant impact on patients, payers, and providers in the coming months and years. The impact is likely going to be felt for some time, and it is a major factor in the rapid transformation going on within the health sector.
8 ways deferred care will impact healthcare
The following is a look at eight ways deferred care will impact healthcare going forward.
1. Lower rates of early detection
In anticipation of COVID-19 treatment needs, healthcare providers have prioritized more emergent and urgent care. Fewer resources have been dedicated to preventative care, early detection of conditions, and elective procedures. Patients have also opted to delay non-essential care.
Mammograms and colonoscopies are among routine screenings that have been deferred. Combined with a new lower age recommendation for a first colonoscopy (down from 50 to 45), there is a backlog of screenings in the system. Given the influence of early detection on long-term health outcomes, delayed screenings are a major health challenge for patients, providers, and payers.
2. More expensive treatment
Reduced resource requirements and lower costs are key benefits of preventative healthcare. Given the delays in routine preventative care, the potential for longer and more expensive care exists for people who miss out on early detection of cancer and other critical diagnoses.
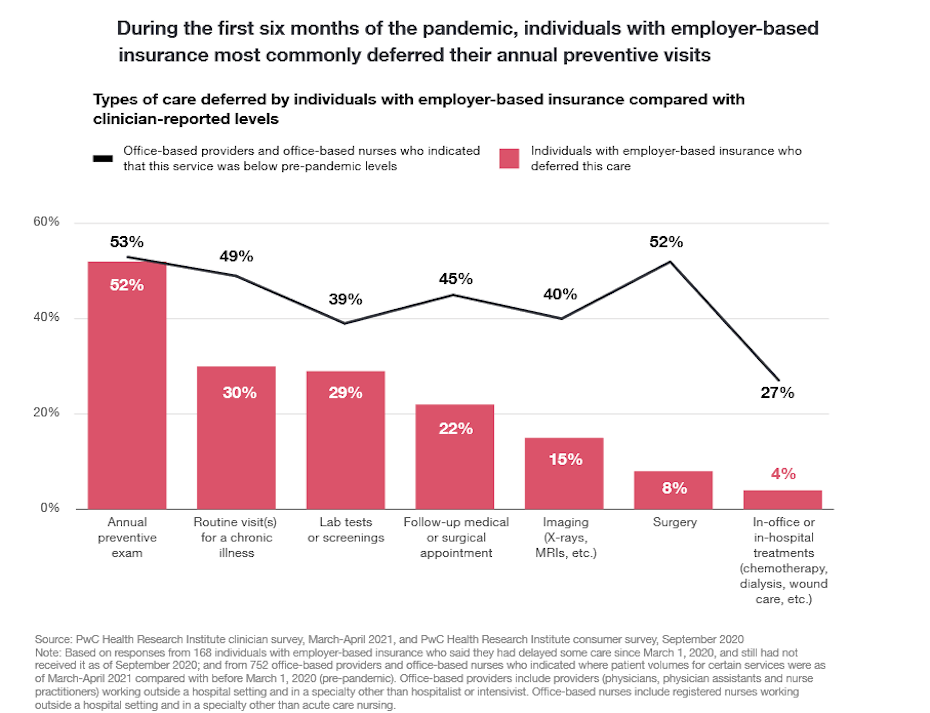
Not only do patients face this burden, but insurers and other payers will feel the crunch as well. As the following chart from PwC illustrates, people on employer-based insurance plans have been more prone to defer care.
3. Scheduling challenges
The combination of continuing COVID-19 variants, prioritization of critical care, and deferred care demands create scheduling challenges. Patients calling providers are likely going to face longer lead times for appointments than they have in the past.
People who deferred elective procedures also face the challenge of trying to book appointments. It may take weeks or months to get on the books. Medical practices also feel the pressure of trying to fit in patients requiring care, as practitioners remain taxed on time and energy.
4. Increased mental health and substance abuse demands
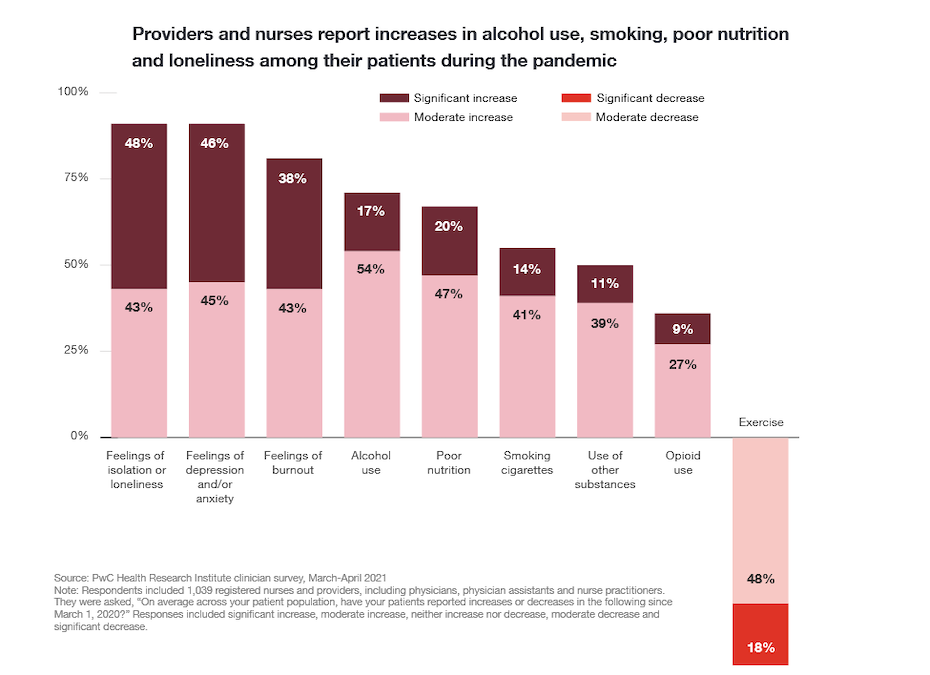
Scheduling challenges apply to mental healthcare as well, given the psychological and emotional burdens created by the COVID crisis. Healthcare providers have reported much higher levels of mental health and substance abuse symptoms among patients, along with poorer nutrition and lower levels of exercise.
As illustrated in the following chart, 91 percent of providers and nurses reported either a moderate or significant increase in feelings of isolation or loneliness among patients. The same percentage indicated a greater prevalence of patients feeling symptoms of depression or anxiety. Nearly half of respondents in both cases stated the increase has been “significant.”
The combination of delayed care, poor nutrition, and reduced exercise compounds the physical and mental health demands putting pressure on the healthcare system.
5. More use of data and targeted communication
There is great demand for effective communication to target populations that have deferred care. In particular, providers and payers need to reach out to people that have deferred important screenings or elective care, while also contacting those now due for screenings. This type of proactive communication represents a transformation for payers and providers that aren’t used to relying on such measures to attract patients.
To achieve cost-effectiveness and efficiency, payers and providers need to rely more on data and predictive analytics to optimize their investments in promotional messaging. The primary objective is to cut off health deterioration among the most affected populations. Along with targeting the right people, choosing the right media and messaging strategies are essential to motivating patients to seek deferred care.
6. More remote workforce
COVID forced many employers to transition into a more remote workforce. Healthcare providers limited on-site staff to those essential to carrying out in-person care. Now that the structure is in place for a more remote workforce, a lot of healthcare providers have made this change permanent.
In addition to some cost advantages, remote workers offer flexibility and agility benefits. Weather conditions and other factors that contribute to workplace absences are often eradicated with remote employees. The pool of potential administrative and support employees is also larger when remote work options are available.
7. Rapid digital investment
To reduce costs, empower a remote workforce and optimize the patient experience, healthcare providers have rapidly invested in digital infrastructure. Patients demand access to multi-channel support access. They want to connect with your agents in a variety of ways at any given time.
Your contact center workforce also needs a unified system for handling a high volume of support inquiries across various channels. Without a robust digital solution, silos create inefficiencies and frustration for your employees and patients. You need a unified solution that allows live agents to manage a cross-channel queue, with access to a patient’s contact history regardless of the channel.
8. Higher healthcare costs
Higher overall healthcare costs are a result of some of the other implications of deferred care mentioned here. Patients and insurers will experience higher costs as a result of the lower rates of early disease detection.
As insurance payouts rise, so too will individual and group premium rates. Providers will have to invest in new equipment, technology, and people to keep up with the demands of COVID and deferred care.

UP NEXT: RingCentral Connect 2021: Using collaboration tools to create the ideal patient experience in healthcare
RingCentral equips payers and providers to succeed
The impact of deferred care is real and it is significant to providers, patients, and payers. Your health plan or practice cannot afford to overlook the items noted here. It is imperative to plan ahead and to equip your workforce with the necessary resources to serve the needs of members and patients.
RingCentral offers a HITRUST CSF-certified cloud communications platform that enables you to keep up with building health service demands and to meet diverse patient and member needs. Getting this type of solution in place is critical to the prevention of communication bottlenecks. Achieve better healthcare outcomes at a lower cost. Cloud-based communications systems are transforming healthcare. Find out how.
Originally published Feb 08, 2022
Looking For Startup Consultants ?
Call Pursho @ 0731-6725516
Telegram Group One Must Follow :
For Startups: https://t.me/daily_business_reads









